Correlation of Norepinephrine with some biochemical Parametric in Patients with type 2 diabetes mellitus.
DOI:
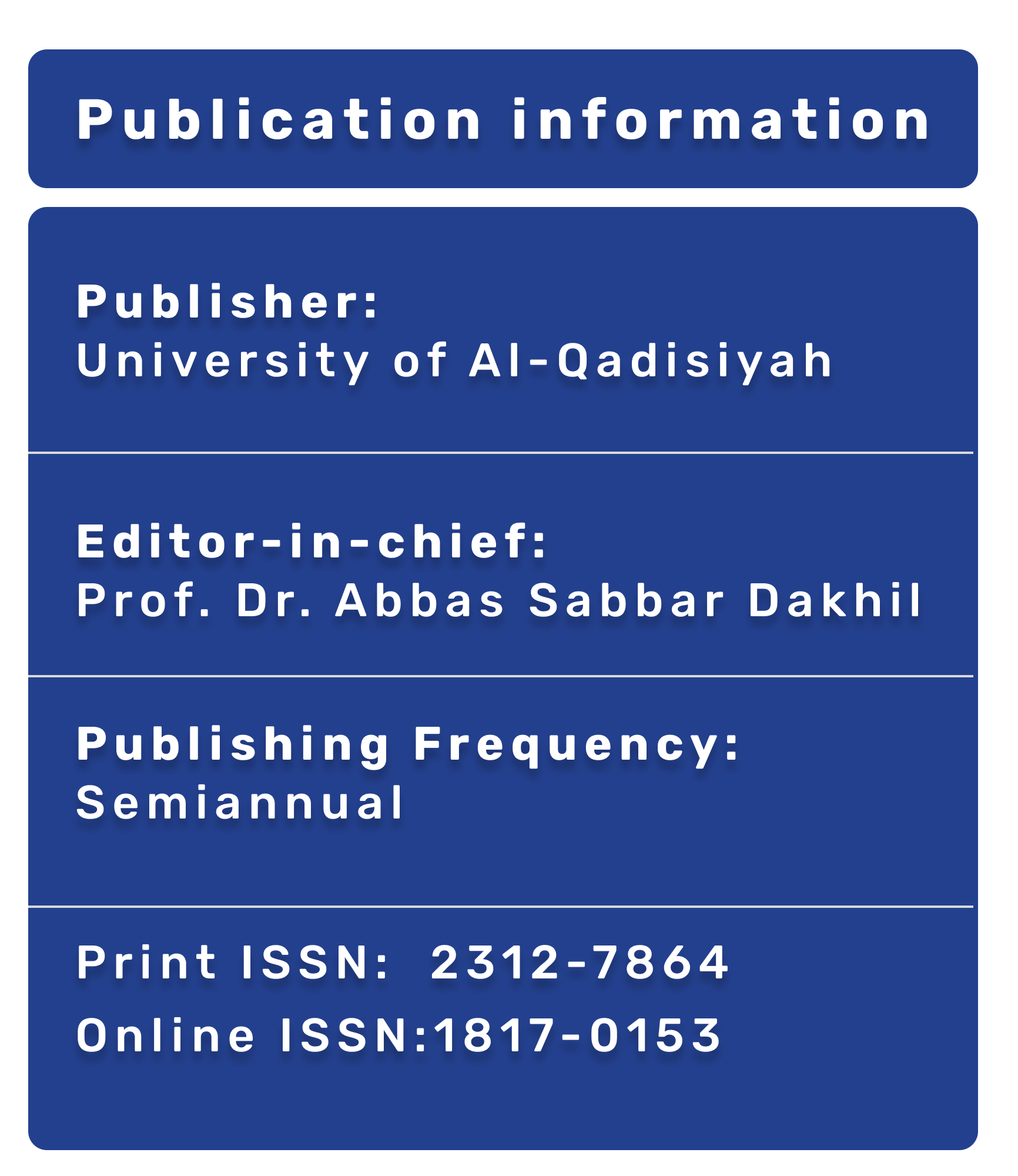
https://doi.org/10.28922/qmj.2023.19.1.15-19Keywords:
NorepinephrineAbstract
Abstract
Background: Type 2 diabetes is a chronic metabolic disorder characterized by high blood sugar levels (hyperglycemia) resulting from the body's reduced ability to produce or use insulin effectively. Insulin is a hormone that regulates blood sugar levels, and in type 2 diabetes, the body either does not produce enough insulin or becomes resistant to its effects. This causes a buildup of glucose in the bloodstream, which can eventually harm organs and tissues. This study was carried out on patients who attended the Diabetes and Endocrinology Specialist Center of Marjan City for Medical Education in Babil Province., all patients were diagnosed by a specialist physician. The practical side of the study was performed at the Clinical Chemistry Laboratory in the College of Medicine and College of Biotechnology, Al-Qadisiyah University.
Objectives: Investigate the Correlation of Norepinephrine with some biochemical Parametric in patients with type 2 diabetes mellitus.
Methods: The method used in this study Enzyme-Linked Immunosorbent Assay (ELISA).
Results: In the metformin treatment group and the group not using antidiabetic treatment, there are weak associations between norepinephrine and insulin levels, but these associations are not statistically significant. In the diamicron MR treatment group, norepinephrine is significantly correlated with lower levels of fasting blood glucose and HbA1c.
Conclusions: Norepinephrine dysregulation may be associated with type 2 diabetes, regardless of specific treatments, indicating a potential role of norepinephrine in the pathophysiology of the disease.
References
Tanase DM, Gosav EM, Costea CF, Ciocoiu M, Lacatusu CM, Maranduca MA, et al. The intricate relationship between type 2 diabetes mellitus (T2DM), insulin resistance (IR), and nonalcoholic fatty liver disease (NAFLD). J Diabetes Res. 2020;2020.
Jansson AK, Chan LX, Lubans DR, Duncan MJ, Plotnikoff RC. Effect of resistance training on HbA1c in adults with type 2 diabetes mellitus and the moderating effect of changes in muscular strength: a systematic review and meta-analysis. BMJ Open Diabetes Res Care. 2022;10(2):e002595.
Zhu Y, Zhang C. Prevalence of gestational diabetes and risk of progression to type 2 diabetes: a global perspective. Curr Diab Rep. 2016;16:1–11.
Galicia-Garcia U, Benito-Vicente A, Jebari S, Larrea-Sebal A, Siddiqi H, Uribe KB, et al. Pathophysiology of type 2 diabetes mellitus. Int J Mol Sci. 2020;21(17):6275.
Faselis C, Katsimardou A, Imprialos K, Deligkaris P, Kallistratos M, Dimitriadis K. Microvascular complications of type 2 diabetes mellitus. Curr Vasc Pharmacol. 2020;18(2):117–24.
Borse SP, Chhipa AS, Sharma V, Singh DP, Nivsarkar M. Management of type 2 diabetes: current strategies, unfocussed aspects, challenges, and alternatives. Med Princ Pract. 2021;30(2):109–21.
Kahn SE, Cooper ME, Del Prato S. Pathophysiology and treatment of type 2 diabetes: perspectives on the past, present, and future. Lancet. 2014;383(9922):1068–83.
Sugama S, Kakinuma Y. Noradrenaline as a key neurotransmitter in modulating microglial activation in stress response. Neurochem Int. 2021;143:104943.
Schwarz LA, Luo L. Organization of the locus coeruleus-norepinephrine system. Curr Biol. 2015;25(21):R1051–6.
Bialik RJ, Smythe JW, Sardelis M, Roberts DCS. Adrenal demedullation blocks and brain norepinephrine depletion potentiates the hyperglycemic response to a variety of stressors. Brain Res. 1989;502(1):88–98.
Sharabi K, Tavares CDJ, Rines AK, Puigserver P. Molecular pathophysiology of hepatic glucose production. Mol Aspects Med. 2015;46:21–33.
Doehner W, Rauchhaus M, Godsland IF, Egerer K, Niebauer J, Sharma R, et al. Insulin resistance in moderate chronic heart failure is related to hyperleptinaemia, but not to norepinephrine or TNF-alpha. Int J Cardiol. 2002;83(1):73–81.
Liu Y, Zhang Y, Xu Q, Yu X, Zhang X, Wang J, et al. Increased norepinephrine by medium-chain triglyceride attributable to lipolysis in white and brown adipose tissue of C57BL/6J mice. Biosci Biotechnol Biochem. 2012;76(6):1213–8.
Tomlinson B, Li Y-H, Chan P. Evaluating gliclazide for the treatment of type 2 diabetes mellitus. Expert Opin Pharmacother. 2022;23(17):1869–77.
Leiter LA, Shestakova M V, Satman I. Effectiveness of gliclazide MR 60 mg in the management of type 2 diabetes: analyses from the EASYDia trial. Diabetol Metab Syndr. 2018;10(1):1–8.
Giorgino F, Laviola L, Eriksson JW. Regional differences of insulin action in adipose tissue: insights from in vivo and in vitro studies. Acta Physiol Scand. 2005;183(1):13–30.
Shurrab NT, Arafa E-SA. Metformin: A review of its therapeutic efficacy and adverse effects. Obes Med. 2020;17:100186.
Streeter CC, Gerbarg PL, Saper RB, Ciraulo DA, Brown RP. Effects of yoga on the autonomic nervous system, gamma-aminobutyric-acid, and allostasis in epilepsy, depression, and post-traumatic stress disorder. Med Hypotheses. 2012;78(5):571–9.
Masuo K, Rakugi H, Ogihara T, Esler MD, Lambert GW. Cardiovascular and renal complications of type 2 diabetes in obesity: role of sympathetic nerve activity and insulin resistance. Curr Diabetes Rev. 2010;6(2):58–67.
Takahashi A, Tabuchi M, Suzuki W, Iizuka S, Nagata M, Ikeya Y, et al. Insulin resistance and low sympathetic nerve activity in the Tsumura Suzuki obese diabetic mouse: a new model of spontaneous type 2 diabetes mellitus and obesity. Metabolism. 2006;55(12):1664–9.
Matthaei S, Bierwirth R, Fritsche A, Gallwitz B, Haering H-U, Joost H-G, et al. Medical antihyperglycaemic treatment of type 2 diabetes mellitus. Exp Clin Endocrinol diabetes. 2009;117(09):522–57.
Sarkar A, Tiwari A, Bhasin PS, Mitra M. Pharmacological and pharmaceutical profile of gliclazide: a review. upset stomach, headache, Ski rash. 2011;(Issue):11–9.
Giannarelli R, Aragona M, Coppelli A, Del Prato S. Reducing insulin resistance with metformin: the evidence today. Diabetes Metab. 2003;29(4):6S28–35.
Tong Y, Xu S, Huang L, Chen C. Obesity and insulin resistance: Pathophysiology and treatment. Drug Discov Today. 2022;27(3):822–30.
Wilcox G. Insulin and insulin resistance. Clin Biochem Rev. 2005;26(2):19.
Inzucchi SE, Maggs DG, Spollett GR, Page SL, Rife FS, Walton V, et al. Efficacy and metabolic effects of metformin and troglitazone in type II diabetes mellitus. N Engl J Med. 1998;338(13):867–73.
Baker C, Retzik-Stahr C, Singh V, Plomondon R, Anderson V, Rasouli N. Should metformin remain the first-line therapy for treatment of type 2 diabetes? Ther Adv Endocrinol Metab. 2021;12:2042018820980225.
Apostolova N, Iannantuoni F, Gruevska A, Muntane J, Rocha M, Victor VM. Mechanisms of action of metformin in type 2 diabetes: Effects on mitochondria and leukocyte-endothelium interactions. Redox Biol. 2020;34:101517.
Zaccardi F, Jacquot E, Cortese V, Tyrer F, Seidu S, Davies MJ, et al. Comparative effectiveness of gliclazide modified release versus sitagliptin as second?line treatment after metformin monotherapy in patients with uncontrolled type 2 diabetes. Diabetes, Obes Metab. 2020;22(12):2417–26.
Martos-Cabrera MB, Velando-Soriano A, Pradas-Hernández L, Suleiman-Martos N, Cañadas-De la Fuente GA, Albendín-García L, et al. Smartphones and apps to control glycosylated hemoglobin (HbA1c) level in diabetes: a systematic review and meta-analysis. J Clin Med. 2020;9(3):693.
Genis-Mendoza AD, González-Castro TB, Tovilla-Vidal G, Juárez-Rojop IE, Castillo-Avila RG, López-Narváez ML, et al. Increased Levels of HbA1c in Individuals with Type 2 Diabetes and Depression: A Meta-Analysis of 34 Studies with 68,398 Participants. Biomedicines. 2022;10(8):1919.
Chehregosha H, Khamseh ME, Malek M, Hosseinpanah F, Ismail-Beigi F. A view beyond HbA1c: role of continuous glucose monitoring. Diabetes Ther. 2019;10:853–63.